Doctors Reveal the Secret Meaning Behind the FVD Medical Abbreviation
Ever seen the abbreviation “FVD” scrawled on a patient’s chart and wondered what it means? In the complex world of medicine, with its alphabet soup of acronyms and abbreviations, deciphering these codes can feel like cracking a secret language. This article delves into the meaning of FVD, exploring its common uses and providing clarity for both medical professionals and those curious about healthcare terminology.
Understanding the FVD Medical Abbreviation: The Basics
The medical abbreviation “FVD” most commonly stands for Fluid Volume Deficit. This term describes a state where the body lacks sufficient fluid, leading to dehydration and potential health complications. Identifying and addressing FVD is crucial in patient care, as it can impact various bodily functions.
Delving Deeper: What Does Fluid Volume Deficit Entail?
Fluid volume deficit signifies a loss of water and electrolytes from the body. This imbalance can result from various factors, including:
- Excessive Fluid Loss:
- Vomiting
- Diarrhea
- Excessive sweating (e.g., during strenuous exercise or in hot environments)
- Diuretic use (medications that increase urine production)
- Hemorrhage (blood loss)
- Reduced Fluid Intake:
- Nausea and vomiting preventing fluid consumption
- Difficulty swallowing
- Inadequate access to fluids
- Unconsciousness
When the body experiences a fluid volume deficit, several physiological changes occur. These can manifest as:
- Signs and Symptoms:
- Thirst
- Dry mouth and mucous membranes
- Decreased urine output
- Dizziness or lightheadedness
- Rapid heart rate (tachycardia)
- Low blood pressure (hypotension)
- Weakness and fatigue
- Concentrated urine (darker color)
- Sunken eyes
- Laboratory Findings:
- Elevated hematocrit (percentage of red blood cells in blood)
- Increased serum osmolality (concentration of dissolved substances in blood)
- Elevated blood urea nitrogen (BUN) and creatinine levels (indicating kidney function)
- Electrolyte imbalances (e.g., low sodium, potassium)
Diagnosing and Treating Fluid Volume Deficit
Healthcare professionals utilize a combination of methods to diagnose and manage FVD:
- Assessment: A thorough patient history, physical examination, and review of symptoms are key. Assessing vital signs (blood pressure, heart rate), skin turgor (skin elasticity), and mental status provides critical clues.
- Diagnostic Tests: Blood tests (electrolytes, BUN, creatinine, hematocrit) and urine analysis help confirm the diagnosis and identify the underlying cause.
- Treatment: The primary goal of treatment is to restore fluid and electrolyte balance. This usually involves:
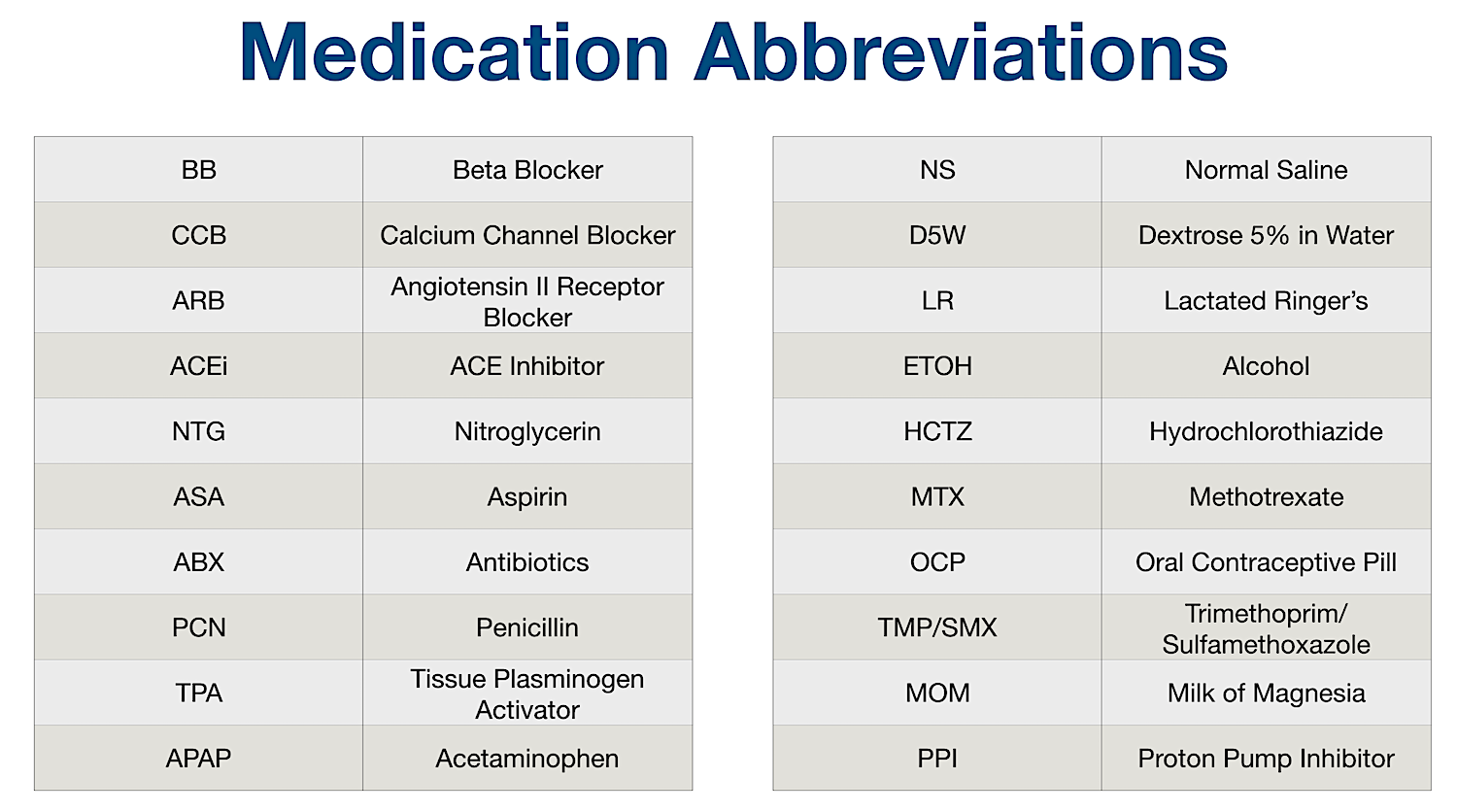
- Oral Rehydration: For mild cases, oral fluids (water, electrolyte solutions) are sufficient.
- Intravenous (IV) Fluids: In more severe cases, IV fluids (e.g., normal saline, lactated Ringer’s solution) are administered to quickly replenish fluids and electrolytes.
- Addressing the Underlying Cause: Treatment focuses on resolving the underlying cause of the fluid loss (e.g., treating vomiting, stopping diuretic use if appropriate).
The Importance of Understanding FVD
Recognizing and treating FVD promptly is vital to prevent serious complications, such as:
- Hypovolemic Shock: A life-threatening condition caused by severe fluid loss, leading to organ damage.
- Acute Kidney Injury: Reduced blood flow to the kidneys can impair their function.
- Electrolyte Imbalances: Can disrupt heart rhythm and other bodily functions.
- Neurological Dysfunction: Dehydration can affect brain function, leading to confusion or altered consciousness.
Understanding the meaning of “FVD” and the potential consequences of fluid volume deficit empowers both healthcare providers and patients to take appropriate action and ensure optimal health outcomes.
Frequently Asked Questions (FAQs)
1. What is the difference between dehydration and fluid volume deficit (FVD)?
While the terms are often used interchangeably, dehydration is a lay term referring to the general state of not having enough fluid in the body. Fluid volume deficit (FVD) is a medical term that describes a specific condition characterized by a loss of both fluids and electrolytes, often with a measurable impact on blood volume and other physiological parameters.
2. What are the most common causes of FVD?
The most common causes include vomiting, diarrhea, excessive sweating, diuretic use, and inadequate fluid intake.
3. How serious is FVD?
The severity of FVD varies. Mild cases may cause only mild symptoms like thirst. Severe FVD can be life-threatening, leading to hypovolemic shock and organ damage.
4. How can I prevent FVD?
Staying well-hydrated is crucial. Drink plenty of fluids throughout the day, especially during hot weather or strenuous activity. Be mindful of potential fluid losses (e.g., during illness) and replace fluids accordingly.
5. Should I be concerned if I see “FVD” on a medical chart?
If you see “FVD” on a medical chart, it indicates that the patient is assessed to have a fluid volume deficit. Discuss your concerns with the healthcare provider for more information about the patient’s condition and the treatment plan.